Mois : octobre 2021
En cours Initiatives
BETTER Women

The BETTER Women Program

The BETTER Program has been successful in helping women initiate healthy lifestyle behaviours to prevent adverse health outcomes. However, it is not feasible to fund Prevention Practitioners to offer repeated follow-up encounters over the period of time needed to turn initial lifestyle behaviour changes into long-term habits. There is growing awareness that lay health coaches can improve and extend the quality and value of primary care. The BETTER Women pilot program is an extension of the BETTER Program, pairing women aged 40-65 with peer health coaches after their initial Prevention Visit. Peer Health Coaches (PHCs) are trained volunteers, who support women over a six-month period to achieve and maintain their health goals.
The pilot program will run for approximately three years (June 2021- August 2024) and is funded by the Public Health Agency of Canada, Canadian Cancer Society and Women’s College Hospital Foundation. The primary objective is to assess whether adding the six-month peer health coaching intervention to the BETTER Program, for women aged 40-65, leads to a greater achievement of evidence-based targets for chronic disease prevention such as decreased smoking, increased activity as well as cancer screening.
The BETTER Women Program will comprise the following stages:
- Design. A PHC Training Program was developed by experts and a team at the Canadian Cancer Society, with input from research team members with expertise in similar programs. The program was competency-based and designed to prepare volunteers to be PHCs with the knowledge, skills, and confidence necessary to use motivational interviewing techniques and brief action planning to support behaviour change. The Canadian Cancer Society is currently facilitating the recruitment and training of volunteers to become PHCs. To be eligible, volunteers must be a woman between the ages of 40-65 years; have experience achieving at least one of the evidence-based behaviours under evaluation, comfortable using computers and the Internet; able to attend PHC training sessions and commit to volunteering three to four hours a week; and able to read, write and speak English. Volunteers for the Summerville Family Health Team site will also be required to self-identify as South Asian and able to speak English. A subset of volunteers will also be able to speak other South Asian languages that are common within the Summerville Family Health Team, such as Punjabi, Hindi, or Urdu. Volunteers meeting screening and eligibility criteria will participate in the custom designed PHC training program before being matched to a patient to provide coaching.
- Implementation. BETTER Women will be implemented at three primary care clinics in Ontario: Women’s College Academic Family Health Team (a large urban academic, hospital-based clinic), Summerville Family Health Team (a suburban clinic where the intervention will focus on the South Asian population), and Barrie and Community Family Health Team – Family Medicine Teaching Unit (a large clinic with a greater proportion of patients from rural areas).Women aged 40-65 will be invited to participate in the BETTER Women pilot program during their Prevention Visit with a Prevention Practitioner. Interested women will be sent information on the program via mail and email. If a woman decides to participate, she will complete a baseline survey with questions about her health and health behaviours. Once completed, she will be randomized to one of two groups: the intervention group or the wait-list control group. More information about recruitment and eligibility can be found on https://clinicaltrials.gov/ct2/show/NCT04746859. Participants in the control group will be matched to a PHC 12 months post-enrollment. Participants in the intervention group will be matched to a PHC right away. Once matched to a peer health coach, participants will have weekly coaching sessions with their peer health coach in months one to three, and monthly coaching sessions in months four to six. Coaching sessions can occur through a variety of methods including phone, email, video calls, or text messaging. Frequency of coaching sessions may vary based on participant needs.
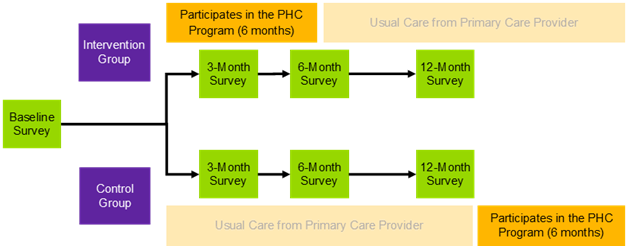
- Evaluation. Several aspects of the program will be evaluated, including the PHC training, program effectiveness and implementation. Evaluation of the PHC training program will include pre- and post-training surveys, as well as focus groups with PHCs to assess the feasibility, acceptability, and effectiveness of the training in preparing PHCs for their role. Program effectiveness and implementation will be evaluated through the BETTER Women trial: a three-site, pragmatic, wait-list controlled, randomized, Type 1 hybrid effectiveness-implementation trial with blinded outcome collection after 12 months. Outcome data will be collected via surveys and chart reviews. The success of the program will be assessed by comparing the number of women in each group who, from baseline to 12-month follow-up, increase the number of targeted actions completed for chronic disease prevention and cancer screening. The multi-method, embedded process evaluation will examine the program’s sustainability, acceptability, cost effectiveness, and other factors that might affect future spread and scale. Data sources for implementation outcomes will include program data, participant surveys, and qualitative interviews with participants, prevention practitioners and PHCs.
For general questions about the BETTER Women program, please contact BETTERWomen@cancer.ca. For questions about the BETTER Women Evaluation please contact BETTERWomen@wchospital.ca.
