Completed Initiatives
BETTER HEALTH: Durham Study

The BETTER HEALTH: Durham study, jointly funded by CIHR and the Canadian Cancer Society, is a study that extends the BETTER Program approach. It consists of a supportive meeting to review chronic disease prevention and screening (CDPS) between a public health nurse taking on the role of Prevention Practitioner and a participant between 40 – 64 years of age who resides in Durham Region of Ontario.
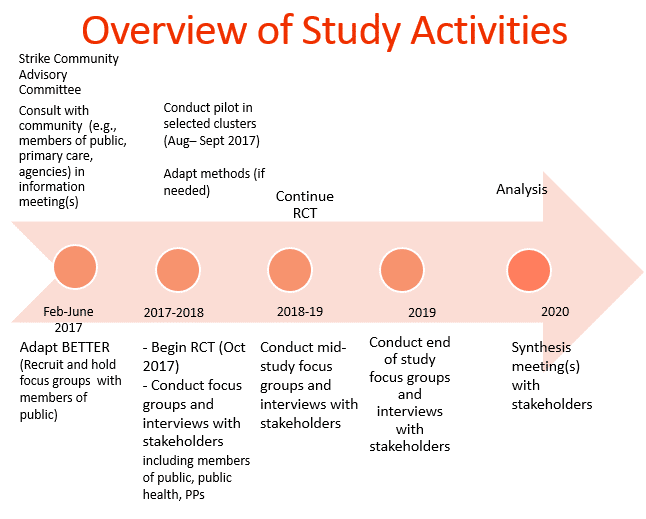
BETTER HEALTH: Durham brings together investigators from Sunnybrook Health Science Centre, St. Michael’s Hospital, Durham Region Health Department and University of Toronto Family & Community Medicine. This project will span from 2017 to 2020.
Our goal with BETTER HEALTH: Durham is to adapt the BETTER intervention guided by community-based participatory research (CBPR) principles. Participants are eligible to participate based on the ‘clusters’ where they reside. Clusters are smaller neighborhoods identified as ‘priority neighbourhoods’ by Durham Health Department, and neighbourhoods where cancer screening uptake is known to be low.
Our first phase was the adaptation phase that spanned February to July of 2017. This included conducting focus groups and one-on-one interviews with members of the public and key informants to review preliminary changes of tools, resources and setting. The linked report reviews 5 themes which resulted from this phase.
The second phase, cluster randomization, will aim to have 5 intervention (immediate) and 5 control (wait-list) clusters with 12 participants in each cluster for a total of 120 participants. The intervention arm participants complete a baseline survey by the research coordinator, complete the prevention practitioner visit and then complete their follow up survey 6 months after. For control participants, they are scheduled for their baseline survey, complete their follow up survey in 6 months and then meet with the prevention practitioner. During the visit with the prevention practitioner, the participants are able to set goals, see where their health is at and be connected to other agencies and resources through the Public Health Nurses’ extensive knowledge of community. Participants have been recruited through many means. Some examples of recruitment strategies include: attending local events, newspaper ads, posting recruitment flyers at various approved agencies and communities, Canada Post mail-out, presentations at agencies, social media etc.
The third phase, a qualitative evaluation will take place with enrolled participants, stakeholders and partners throughout the study, who will be asked to answer a range of questions from their experiences to their thoughts of implementations of the study. The qualitative phase will be based on grounded theory principles and informed by the Consolidated Framework for Implementation Research (CFIR).
Through these phases, we plan to share the adapted BETTER knowledge with a wide range of stakeholders, including policy makers, advisors, public health, primary care, community and national organizations, and with the larger research audience, using the Knowledge Transition (KT) plan.
Below compares the original BETTER study in primary care to BETTER HEALTH: Durham.
| BETTER in primary care practices | BETTER HEALTH: DURHAM | |
| Physical location of prevention practitioner (PP) | In primary care team clinics | Embedded in Health Department, Durham Region, for community outreach |
| Identification of participants | From electronic medical record | Community-based recruitment strategies |
| Identification of completed and current behaviours and activities | From electronic medical record, and from self-report in self-administered survey | From self-report responses to survey administered by research coordinator |
| Identification of risk factors | Lab tests, survey, electronic medical record | Self report |
| Motivational interview by PP and goal-setting by participants | By prevention practitioner in primary care team clinics | By prevention practitioners at various community locations |
| Facilitation of goal achievement | Clinic staff, prevention practitioner, links, and self | Prevention practitioners, links, and self |
| Strategy to find primary care physician for participants. | Not applicable | Prevention practitioners supported by primary care strategy engaging physicians and clinics near the clusters. |
| Primary outcome measures | Composite index, expressed as the ratio (multiplied by 100) of the number of eligible CDPS (chronic disease prevention and screening) actions at baseline (denominator) that were subsequently met at follow-up (numerator), measured at the patient level. (G*) | |
| Ascertainment of outcomes | Abstraction from EMR and self-report responses at repeat self-administered survey by prevention practitioner | Self-report responses to survey administered by research assistant |
For more information about the BETTER HEALTH: Durham study, please contact Dr. Lawrence Paszat at LawrencePaszat@sunnybrook.ca
