Completed Initiatives
The BETTER Trial

The purpose of the BETTER Trial was to determine whether prevention and screening for cancer and other chronic diseases such as diabetes and heart disease could be improved in the family practice setting.
BETTER was a pragmatic cluster randomized controlled trial (RCT) predicated on the Ontario Ministry of Health and Long Term Care’s Chronic Disease Prevention and Management Framework.
The setting for the BETTER Trial was eight, urban, Primary Care Team (PCT) practices in two Canadian jurisdictions (Toronto, Ontario and Edmonton, Alberta). PCTs are integrated primary care delivery models that include an inter-professional team. They work collaboratively to provide comprehensive, accessible, and coordinated primary healthcare to their rostered patients. The team typically comprises a combination of primary care physician (PCP), nurse practitioner, nurse, dietitian, pharmacist and other healthcare professional members.
Eight PCTs participated in BETTER, 4 in each jurisdiction, and 4 primary care physicians (PCPs) within each PCT participated as well, for a total of 32 PCPs (16 in each jurisdiction). Two PCTs in each jurisdiction were randomly allocated to the practice-level intervention arm. Within each PCT, two of the four participating Primary Care Physicians (PCPs) were randomly allocated to the patient-level intervention arm, for a total of 16 PCPs between both jurisdictions.
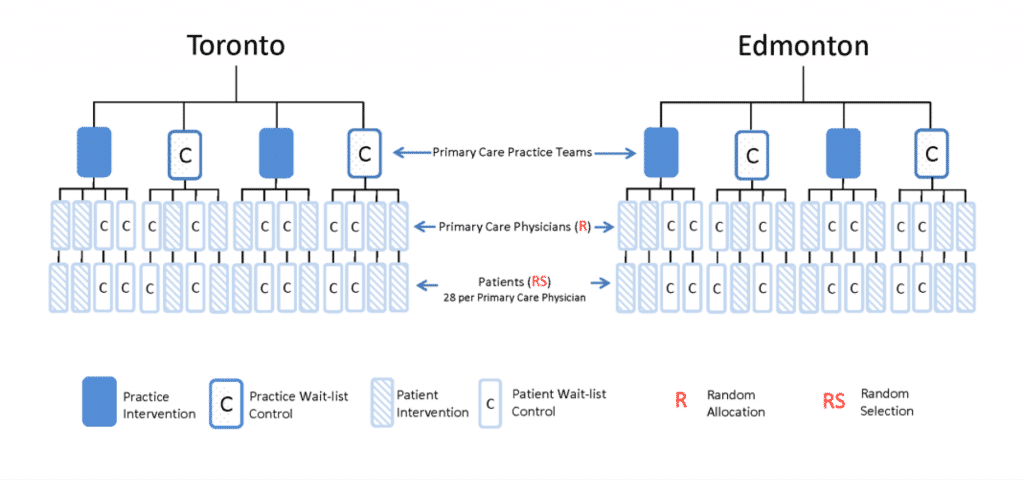
Therefore, the two-way factorial design produced:
- Eight PCPs whose patients received the practice-level intervention only;
- Eight PCPs whose patients received the patient-level intervention only;
- Eight PCPs whose patients received both the practice-level and patient-level interventions;
- Eight PCPs whose patients and practice continued to receive usual care.
Patient-level Intervention – Internal Facilitation
The patient-level facilitation intervention involved 8 Prevention Practitioners (1 per PCT), who were healthcare professionals available within each PCT and chosen by the practice to undertake the role. The Prevention Practitioners received specialized training in the BETTER approach to evidence-based prevention and screening maneuvers and was responsible for meeting with patients one-on-one to assess their risk for chronic disease and helping them set chronic disease prevention and screening (CDPS) goals (i.e. the “Prevention Visit”). Through shared decision-making, the Prevention Practitioner and the patient developed a “Prevention Prescription” tailored specifically to that patient based on their medical and family history, and chronic disease risk. This personalized Prescription may have included referrals for screening procedures and/or referrals for lifestyle modification programs as appropriate.
Practice-level Intervention – External Facilitation
The practice-level facilitation intervention involved 2 Practice Facilitators (1 per jurisdiction), who were individuals from outside the practice, trained in the BETTER approach to CDPS. Each Practice Facilitator was trained by the Centre for Effective Practice (CEP) and Quality Improvement and Innovation Partnership (QIIP) to work with representatives of each PCT to develop CDPS care paths for each maneuver used in BETTER. Each Practice Facilitator assessed the practices’ use of their electronic medical record (EMR) and prepared a “Prevention Prescription” aimed to better enable the EMR for CDPS (e.g. patient invitation letters, audit and feedback, decision support) and tailored to the needs of each PCT, with a focus on optimizing the use of information tools and resources available to the practice.
BETTER Results
Recruitment for BETTER started in August 2010 and ended in March 2011, resulting in the enrollment of 789 patients aged 40-65. Analysis shows a strong positive effect of the patient-level facilitation intervention and a minor effect of the practice-level facilitation intervention.
Several outputs were also generated as a result of the BETTER Trial:
- Evidence-based care paths for each chronic disease prevention and screening maneuver, including tools and a toolkit tailored to the primary care setting;
- The BETTER algorithm, which is a useful tool to inform clinicians on how to approach chronic disease prevention and screening; and
- Patient education and motivational interviewing tools that aid clinicians in their assessment of each patient’s individual risks for chronic disease and the patient’s readiness to change.
More information about the BETTER cluster randomized controlled trial, can be found in our publications section.
The BETTER trial was made possible through a financial contribution from Health Canada, through the Canadian Partnership Against Cancer’s Coalitions Linking Action & Science for Prevention (CLASP) initiative, and from the Heart and Stroke Foundation of Canada.

The BETTER Trial Team (2009 – 2012)
Principal Investigators: Dr. Eva Grunfeld and Dr. Donna Manca
Methodology Working Group: E. Grunfeld (Chair), D. Manca, R. Moineddin, K. Thorpe, M. Mamdani, P. Krueger.
Clinical Working Group: D. Campbell-Scherer (Chair), R. Barrett, S. Bell, S. Bible, S. Buchman, J. Carroll, M. Dhaliwal, S. Dunn, M. Griever, E. Grunfeld, C. Harrison, L. Hosford, M. Kahan, D. Klein, C. Korownyk, K. Lang-Robertson, D. Manca, J. Meuser, V. Mozgala, J. Pencharz, L. Radmanovich, J. Rogers, G. Salvalaggio, L. Schaar, R. Stoller, D.L. Vesik, R. Wymer, M. Yan.
Statistical Analysis: R. Moineddin, K. Thorpe, C. Meaney.
Trial Coordination: Applied Health Research Centre, L. Patterson, C. Fernandes.
Economic Analysis: J. Hoch, J. Beca.
Research Assistants: T.K. Dallman, K. Kam, M. Leyland, P. Patel, D. Sanderson, C. Wright.
